Hi, Baobao, I learned much from your steady approach to tackling the HBV. Is this something related to your approach?
Slide 11. Treatment Options
Some of these same variables turn out to be important with pegylated interferon, although it has not been addressed as decisively as it has been for the standard interferon trials.
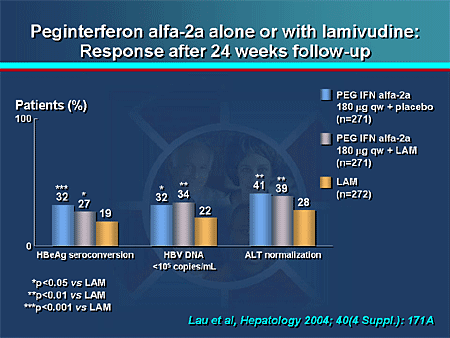
Slide 12. Peginterferon Alfa-2a Alone or With Lamivudine: Response After 24 Weeks Follow-up
The first set of bars here are pegylated interferon alone. The second bars are pegylated interferon, with lamivudine not showing any added benefit. The third set of bars are lamivudine alone. One of the important variables that came out is that HBeAg-positive patients, patients who have genotype A, respond significantly more frequently than patients with genotype D. Genotypes B and C have intermediate levels of response. A good way of remembering this is that it follows the alphabet -- A is better than B is better than C is better than D. Pegylated interferon is also more antiviral, causing about a 4-log reduction at the end of 48 weeks of therapy, which gets in the range with some of the first-generation nucleoside analogs. Very little has actually been made of pegylated interferon's immunomodulatory benefit. However, if you look carefully at the studies, you will see that people who had on-treatment flares of ALT tended to respond more frequently.
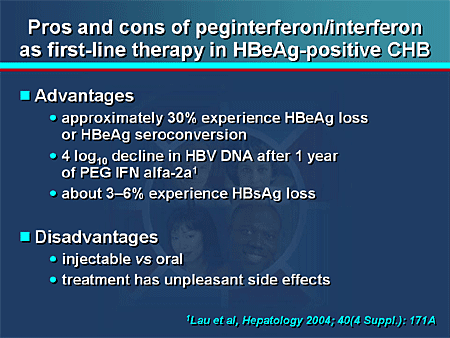
Slide 13. Pros and Cons of Peginterferon/Interferon as First-line Therapy in HBeAg-Positive CHB
The pros and cons of pegylated interferon are obvious to many of us. It comes down not so much to cost, particularly when you are comparing it with long-term nucleoside analog therapy. The HBsAg loss is nice to see, but it occurs in a small minority of treated patients. It comes down to the disadvantages of the side-effect profile of interferon. This does not mean that we should not be using it. It means that we should carefully select the patient in whom we think it might be tolerable.
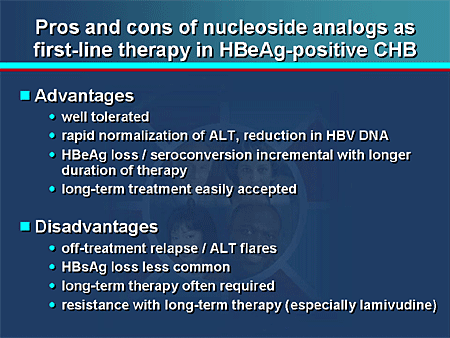
Slide 14. Pros and Cons of Nucleoside Analogs as First-line Therapy in HBeAg-Positive CHB
Nucleoside analogs are extremely well tolerated and have allowed us to go ahead with long-term therapy. As drugs have come along with lower and lower resistance rates, we are even more successful in being able to apply this long-term therapy to maximize our gains. The disadvantages are that if you stop the therapy, you may run into some treatment flares in about 20% to 25% of patients. It will be interesting to see if we see the same type of correlates with the more potent nucleoside analogs that are being developed, such as entecavir. HBsAg loss is less common. However, with prolonged therapy, there is incremental gain, and HBsAg loss has been repeated, although it is not at the level that we see with interferon. Long-term therapy is often required